Breathing shapes sleep, mood, and stamina, so a deviated septum is more than a cosmetic concern. If you are weighing nasal deviation surgery, begin with clear goals and real-world tests rather than impulse fixes. A consultation with an ENT doctor sets a baseline, aligns expectations, and maps risks that matter for recovery.
1. Map Your Symptoms Across 24 Hours
Write down how congestion, mouth breathing, and snoring change from morning to night. Note exercise tolerance, headache timing, and how often you reach for decongestants. Bring this log to the clinic so your ENT doctor can link complaints to anatomy and lifestyle, not just what the camera sees.
2. Separate Structure from Inflammation
A bent septum narrows airflow, while swollen turbinates and sinus lining add a second layer of blockage. Ask for a stepwise plan that includes saline rinses and medical therapy before committing to nasal deviation surgery. If medicines improve comfort but airflow stays poor, structure is likely the main driver.
3. Test Real Life, Not Just Clinic Numbers
Data should predict daily comfort. Walk briskly for six minutes and record perceived effort through each nostril; repeat after a decongestant trial. Track sleep quality with a simple app. These low-tech tests help your ENT doctor judge whether structural correction would change how you live, not only how you look.
4. Align Surgery with Work, Sport, and Caregiving
Recovery is short for most patients, yet timing still matters. Check project deadlines, childcare, and training cycles, then choose a fortnight with lighter demands. Planning reduces the urge to ignore post-operation advice and protects the healing lining so results last.
5. Ask About Anaesthesia, Technique, and Scarring
Clarify whether your case suits septoplasty alone or combined with turbinate reduction. Confirm anaesthesia type, expected swelling, and visible marks. In most cases, nasal deviation surgery reshapes the midline internally, so external scarring is minimal; a calm briefing keeps expectations realistic.
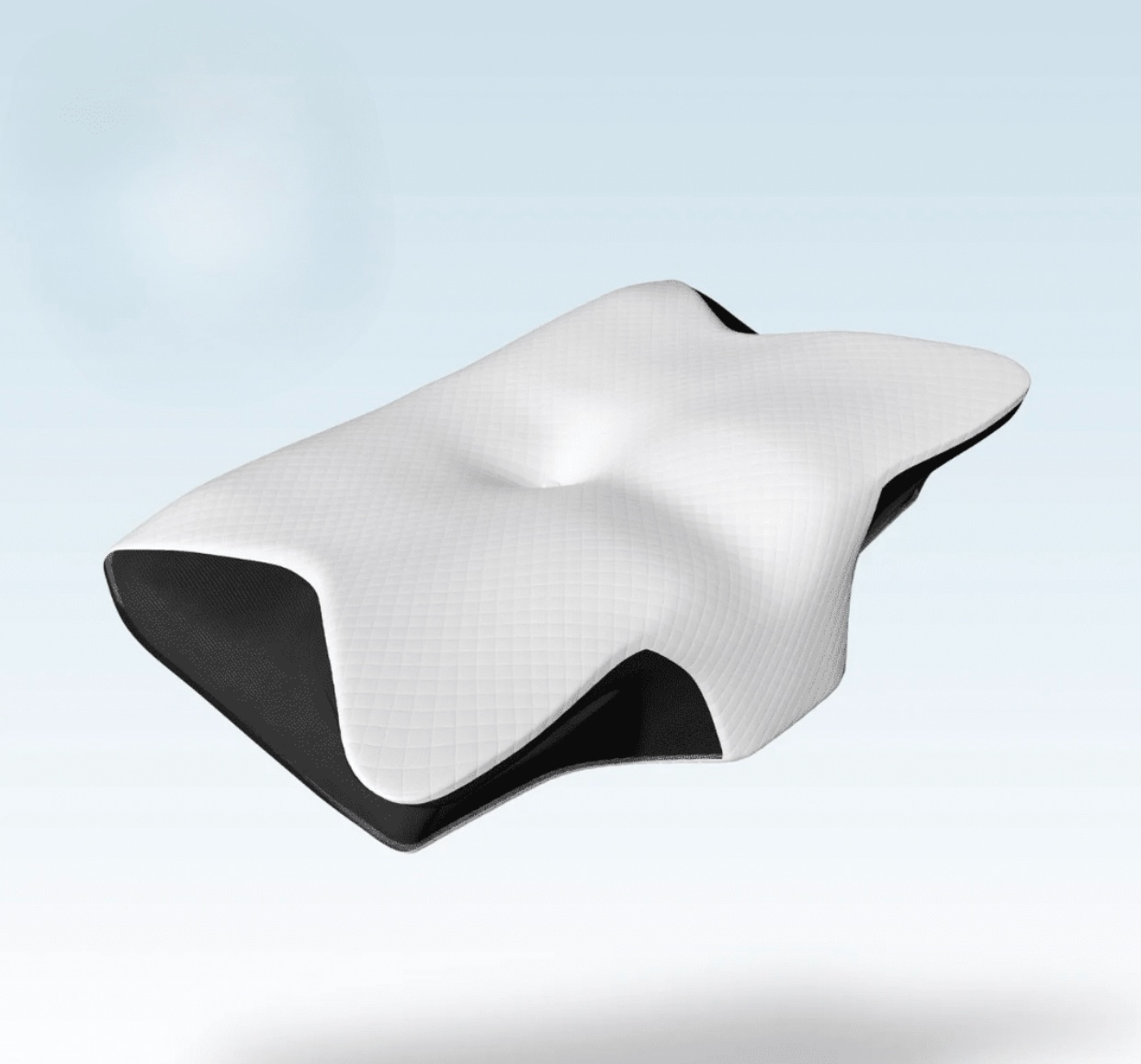
6. Plan for Comfort in the First Week
Stock saline, a gentle pain reliever, and a cool gel pack for short intervals. Sleep head-elevated on two pillows and avoid nose blowing. Switch to easy meals. Small comforts shorten recovery and reduce the risk of bleeding or crusting.
7. Protect Sleep While You Heal
Good sleep speeds repair. Use a humidifier if the air feels dry, and keep pets out of the bedroom to limit dander. Avoid alcohol until your follow-up because it worsens swelling. Most people resume gentle activity within days; confirm your timeline with the ENT doctor who operated.
8. Rebuild Fitness Gradually
Return to walking first, then add low-impact cardio. Postpone heavy lifts and contact sports until cleared at review. Breathing should feel steadier week by week; if one side still collapses, ask about physiologic nasal valve support rather than forcing early intensity.
9. Measure Success with the Same Tools You Started
Repeat the six-minute walk test, the sleep notes, and the decongestant comparison. If objective gains match how you feel, you made a good call. If gaps remain, your clinician can refine allergy care or adjust timelines further.
10. Plan for Air Travel and Allergies
If you fly often, schedule surgery outside peak travel to avoid cabin pressure discomfort. Review allergy triggers and start avoidance and medical control before and after the procedure. Stable lining reduces swelling and helps the structural gain from nasal deviation surgery feel obvious in everyday air.
11. Know Costs, Coverage, and Time Off
Verify the company’s medical leave policy and request a detailed estimate that breaks down the costs for the surgeon, the facility, and the anaesthesia. Clarify which reviews are included and when out-of-pocket charges apply. Clear numbers prevent last-minute stress and let you focus on healing.
Conclusion
Choices feel easier when you test, plan, and measure. With a clear log, a staged medical trial, and honest functional goals, nasal deviation surgery becomes a practical decision rather than a leap. Maintain consistent progress throughout the season by closely monitoring your ENT physician.
For evidence-based assessment, clear surgical planning, and attentive follow-up, contact Dr. Leslie Koh.